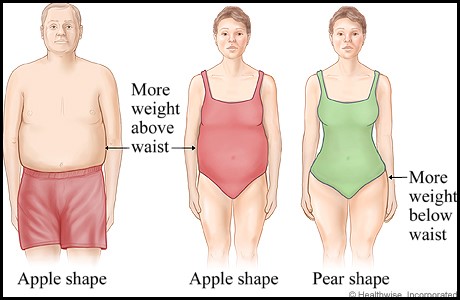
Where you store your fat is almost as important as how much body fat you have overall. As I have mentioned in numerous blogs, body fat acts as active biological tissue. It releases hormones and increases the risk of various diseases. There are two shapes defined by the location of fat storage: apple and pear-shaped. Apple-shaped people store fat around their midsection and waist. Think of older men with huge, protruding stomachs. Pear-shaped people store fat around their hips, thighs, and buttocks and less around their waist. Many women fit this description.
Which shape is worse? Apple shaped. Storing fat around your organs is more dangerous than storing fat around your thighs and buttocks. At least, that is what most research shows. Common sense would lead you to believe that fat in a place like your arm is a lot less dangerous than fat around your organs. But common sense often fails us. In this blog, I will talk about research showing that apple-shaped fat (visceral fat) is metabolically different from pear-shaped fat (subcutaneous fat) and that both types increase the risk of various diseases.
A few reminders
- In this blog, adipose tissue and body fat are considered the same thing.
- Remember- apple shaped people store fat around their organs and in their stomach. This is mostly visceral fat. Pear shaped people store fat around their hips and thighs, and less around their waist. This is mostly subcutaneous fat, which makes up about 90% of our overall fat mass.
- For most of the blog I will abbreviate visceral fat as VAT-visceral adipose tissue, and subcutaneous fat as SAT-subcutaneous adipose tissue.
- VAT = around organs. SAT = under the skin.
- Waist circumference is used as an indicator for levels of visceral fat.
As men age visceral fat area increases
Usually, men have more visceral fat than women, even when matched by age and sex. Also, as men age, their levels of visceral fat increase more than are seen in women.
Metabolic differences between visceral (VAT) and subcutaneous fat (SAT)
Blood Pressure
- Circulatory system – consisting of the heart, blood vessels, blood, lymph, and the lymphatic vessels and glands.
Abdominal obesity increases the risk of circulatory system disease by raising blood pressure. Abdominal obesity may cause hypertension by affecting hormones responsible for maintaining salt-fluid homeostasis (when this balance is changed, our blood pressure can change). Fat cells of obese people with high levels of abdominal fat produce angiotensin (AGT) and angiotensin II (hormones closely linked to blood pressure), which lead to increased blood pressure levels. A reduction in waist circumference is associated with a 7 mmHg (point) decrease in systolic blood pressure.
Heart disease and changes in lipids
The Jackson Heart Study, involving almost 2500 subjects, measured the effect of subcutaneous and visceral fat on heart disease risk (1). The researchers found that both subcutaneous fat and visceral fat were associated with higher blood pressure readings, triglyceride levels, and fasting plasma glucose (blood sugar), but decreased HDL (good cholesterol) levels. Although both types of adipose tissue increased the risk of heart disease, visceral fat was associated with a greater risk than subcutaneous fat.
Insulin resistance
In a very large study called the Framingham Heart Study, researchers measured the relationship between visceral fat, subcutaneous fat, and insulin resistance (2). The study found that levels of visceral and subcutaneous fat were associated with insulin resistance and high insulin levels, but the association was stronger for visceral fat. Insulin resistance often leads to type II diabetes. The results of this study are particularly significant because of the large sample size (3,000 participants), since only a handful of the previous studies on this topic had more than 100 subjects.
Type II Diabetes
It is common knowledge for most that obesity greatly increases the risk of type 2 diabetes. Although how obesity causes type II diabetes is likely multifactorial, one theory involves beta cells. Beta cells are found in the pancreas and are responsible for storing and secreting insulin. Obesity may cause beta cell dysfunction by increasing the mass of the beta cells. The release of fatty acids by visceral fat cells leads to the expansion and dysfunction of beta cell mass and an increased risk of diabetes. Keep in mind that this is just a theory and may or may not be correct. Either way, it is still an interesting theory that deserves further study.
Inflammation
- Adipocytokines- a general term for a bioactive product produced by adipose tissue (fat tissue). Includes inflammatory markers.
- Macrophages- immune system cells that respond to infection. Inflammation often leads to the mobilization and build up of macrophages in the inflamed area.
There are a few inflammatory markers that adipose tissue creates and releases. The main ones are TNF (tumor necrosis factor), IL-6 (interleukin 6), CRP (C-reactive protein), and adipsin (3). High IL-6 levels are associated with insulin resistance, a higher risk of diabetes, and vascular inflammation. The fat cells of obese subjects contain more macrophages than the fat cells of lean subjects, which increases the risk of insulin resistance. TNF increases vascular inflammation and decreases insulin sensitivity. Studies have shown that waist circumference and visceral fat are strongly correlated with levels of C-reactive protein.
Obesity is marked by a chronic, low-inflammatory state, which over time leads to many metabolic disorders. This inflammatory state partly results from changes in the function of fat cells and macrophages. Therefore, obesity is marked by a dysfunction of adipose tissue. The adipose tissue associated with obesity hypersecretes pro-inflammatory, pro-diabetic, and pro-atherogenic (the buildup of plaque in the arteries) adipocytokines. SAT has smaller adipocytes than VAT. Smaller adipocytes are more sensitive to insulin. Larger adipocytes in VAT are more dysfunctional.
VAT discharges into the portal vein
- Portal vein- vein delivering blood to the liver
The main hypothesis for VAT being metabolically worse than SAT, is that VAT drains into the portal vein, which goes to the liver (4). I say hypothesis because it is merely a theory explaining metabolic changes but we are not certain that this is the cause. When excessive cholesterol goes from VAT into the liver, the liver changes LDL cholesterol (bad cholesterol) into small and dense LDL cholesterol, which contributes to hardening and plaque in the arteries. The liver processes blood, detoxifies harmful substances, metabolizes nutrients and much more. When you have excessive fat cells going from VAT directly to the liver, you can negatively affect the way the liver works.
Metabolic risk associated with fat location
Researchers used subjects from the Framingham Heart Study to find the association between subcutaneous fat and visceral fat and metabolic risk (5). There was a significant correlation between all metabolic risk factors and both SAT and VAT. In women, both SAT and VAT showed similar effects on raising blood pressure. In men, VAT was associated with slightly higher blood pressures than SAT. For fasting glucose, both SAT and VAT showed similar effects. Both SAT and VAT were associated with higher levels of hypertension, although the effect was slightly higher with VAT. Both SAT and VAT were associated with low HDL levels (good cholesterol) and high triglyceride levels. This study highlights the fact that both SAT and VAT increase the risk of metabolic disorders.
Deep SAT is more similar to VAT than it is to superficial SAT
- Thigh AT – thigh adipose tissue (fat tissue on the thigh)
- Superficial SAT – superficial subcutaneous adipose tissue
- Deep SAT- deep subcutaneous adipose tissue – located deep in the abdomen towards the back
- VAT- visceral adipose tissue
There appear to be two types of abdominal SAT: the superficial layer and the deeper layer (6). The packaging of fat molecules may differ between the two areas. The superficial layer has small, tightly packed lobules, while the deeper layer has larger lobules and a more irregular distribution. A study using a CAT scan aimed to find the metabolic differences between the superficial SAT and the deeper SAT.
For glucose disposal rates (a measure of insulin resistance), as fat mass increased, glucose disposal decreased (bad), although there was no association between thigh AT and superficial SAT. As deep SAT increased, glucose disposal rates decreased, similarly to VAT. For fasting insulin, deep SAT and VAT showed similar correlations, while superficial SAT and thigh AT had similar correlations, which were different than deep SAT and VAT. Both VAT and deep SAT were similar in relation to triglyceride levels and HDL cholesterol, while superficial SAT and thigh AT had a similar relationship, which was different from VAT and deep SAT.
Overall, it was shown that deep SAT behaves more similar to VAT than it does to superficial SAT. It also showed that superficial SAT is similar to thigh AT, and both are less harmful than deeper SAT. This study has important implications for the way that we look at deep subcutaneous adipose tissue. It is important to make the distinction between superficial SAT and deeper SAT, since deeper SAT has similar detrimental metabolic effects as VAT.
We must change the way we look at adipose (fat) tissue
As I mentioned many times in the past, our body fat is not just a place where we store energy for later use. Studies have shown that adipose tissue plays a role in the metabolism of lipids and glucose, and produces hormones and inflammatory markers (3). The release of hormones and inflammatory markers by adipose tissue affect the functioning of many organs, such as our liver, muscles and brain (Adipose tissue dysfunction in obesity, diabetes, and vascular diseases). Activity of our adipose tissue is largely responsible for all of the metabolic diseases associated with obesity.
Conclusion
Any extra body fat increases disease risk. Even though VAT increases disease risk more than SAT, the difference is not that big, and both increase the risk of heart disease, diabetes, and hypertension. I would recommend shedding any extra body fat if possible. Besides affecting disease risk, any extra body fat also puts a strain on our joints, such as the knees. Even though SAT is not directly near our organs, it still produces and releases inflammatory markers and hormones.
Source
- Liu, J., Fox, C. S., Hickson, D. A., May, W. D., Hairston, K. G., Carr, J. J., & Taylor, H. A. (2010). Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. The Journal of Clinical Endocrinology & Metabolism, 95(12), 5419-5426.
- Preis, S. R., Massaro, J. M., Robins, S. J., Hoffmann, U., Vasan, R. S., Irlbeck, T., … & Fox, C. S. (2010). Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obesity, 18(11), 2191-2198.
- Hajer, G. R., van Haeften, T. W., & Visseren, F. L. (2008). Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. European heart journal, 29(24), 2959-2971.
- Ibrahim, M. M. (2010). Subcutaneous and visceral adipose tissue: structural and functional differences. Obesity reviews, 11(1), 11-18.
- Fox, C. S., Massaro, J. M., Hoffmann, U., Pou, K. M., Maurovich-Horvat, P., Liu, C. Y., … & D’Agostino, R. B. (2007). Abdominal visceral and subcutaneous adipose tissue compartments association with metabolic risk factors in the Framingham Heart Study. Circulation, 116(1), 39-48.
- Kelley, D. E., Thaete, F. L., Troost, F., Huwe, T., & Goodpaster, B. H. (2000). Subdivisions of subcutaneous abdominal adipose tissue and insulin resistance. American Journal of Physiology-Endocrinology And Metabolism, 278(5), E941-E948.




What an interesting post Rob!
I agree with Bernal, very interesting blog.
The reminders at the begging of the article made the reading easier.
Keep it up Rob! Great work.